at Grand Health Partners
“Do I really have to live with frequent heartburn, acid reflux, or GERD?
This is a common question that our providers hear. The answer is: “NO!”
At the Grand Health Partners GERD clinic, we are experts in treating reflux disease. If you’re suffering from heartburn, acid or bile reflux or GERD, schedule an appointment today to determine the best treatment plan for you!
Heartburn, Acid Reflux, Bile Reflux and GERD (Gastroesophageal Reflux Disease) are related conditions that involve the back flow of stomach contents including food, stomach acid and/or bile into the esophagus. Reflux can cause discomfort, irritation and long-term damage that can result in serious medical conditions or cancer. GERD treatment focuses on reducing acid reflux through lifestyle changes, medications to control stomach acid, and when appropriate—minimally invasive procedures to address the underlying cause and provide lasting relief.
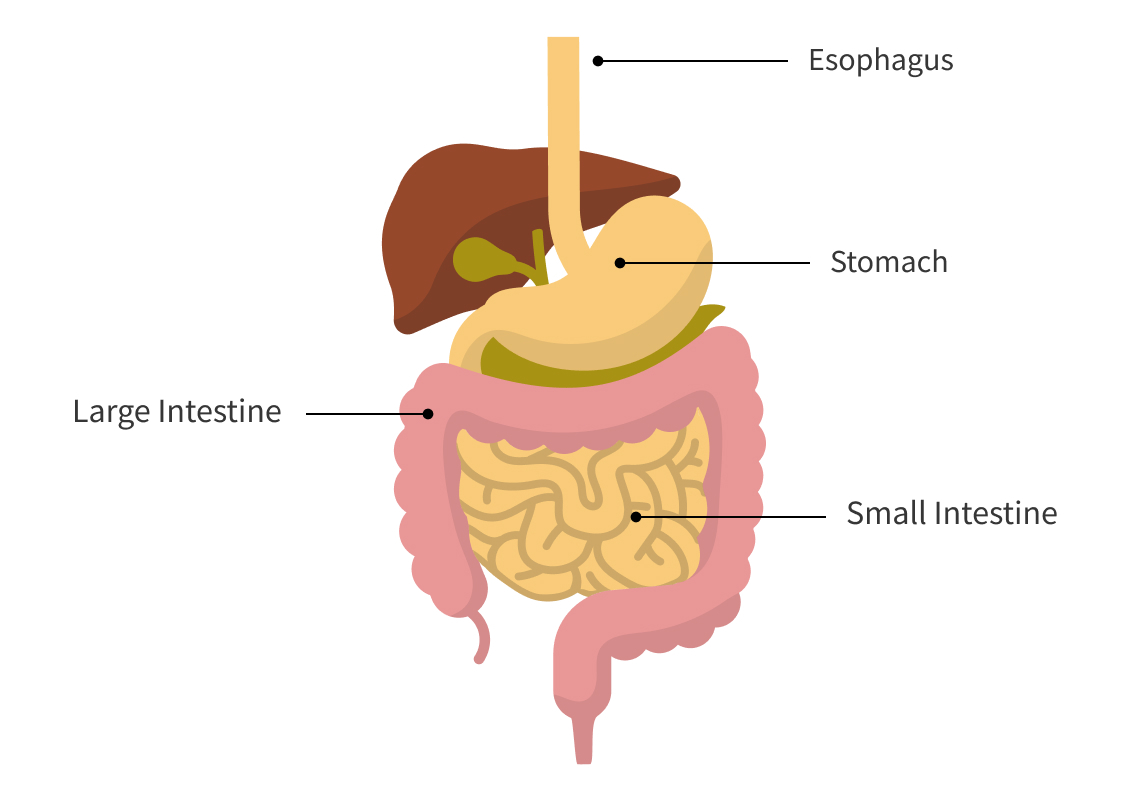
Acid is made in the stomach to help us break down food and kill bacteria. Bile is made and released just after the stomach (in the duodenum) to help us breakdown foods, especially fats. Acid reflux occurs when stomach acid flows backward (refluxes) into the esophagus (the tube that connects the mouth to the stomach). Bile reflux is when the bile backs all the way up to the esophagus. This can happen occasionally in healthy individuals, typically after meals, and is usually temporary and is often called “heartburn”.
Common Symptoms:

is a more severe and chronic (long term) form of acid and bile reflux. It is diagnosed when reflux occurs more than twice a week or when symptoms persist for an extended period, typically lasting for more than three months. GERD can cause more serious complications and discomfort than occasional acid reflux.

Common Symptoms:
Symptoms of GERD are similar to acid reflux but occur more frequently
Complications of Untreated GERD
If left untreated, GERD can lead to more serious health problems, including:
Treatment for Heartburn, Acid Reflux, Bile reflux and GERD typically involves a combination of lifestyle changes, medications, and in some cases, surgery. Lifestyle modifications may include avoiding trigger foods, losing weight, and eating smaller meals. Medications may include antacids, proton pump inhibitors (PPIs), or H2 blockers. Surgical options include fixing hiatal hernias, wrapping the stomach around itself (fundoplication) and surgery to help treat obesity.
The treatment options for GERD (Gastroesophageal Reflux Disease) and Reflux typically involve a combination of lifestyle changes, medications, and in some cases, surgical interventions. The goal is to relieve symptoms, improve quality of life, and prevent complications. Here’s a breakdown of heartburn treatment options offered at Grand Health Partners in Grand Rapids.

Lifestyle Modifications
Schedule a Consultation with our Anti-Reflux Specialists now!
Medications
Several types of medications can help manage GERD symptoms:
Antacids
These neutralize stomach acid and provide quick relief for mild, occasional acid reflux. Examples include Tums, Maalox, and Rolaids.
Pros: Fast-acting.
Cons:
H2 Receptor Antagonists (H2 Blockers)
These drugs reduce the amount of acid the stomach produces. Examples include ranitidine (Zantac) and famotidine (Pepcid).
Proton Pump Inhibitors (PPIs)
PPIs reduce stomach acid production more effectively and are often prescribed for more severe cases of GERD. Examples include omeprazole (Prilosec), lansoprazole (Prevacid), and esomeprazole (Nexium).
Prokinetics
These medications help improve the movement of food and acid through the digestive tract, reducing reflux. Examples include metoclopramide (Reglan).
Bile Acid Sequestration
These medications help bind bile. Example: Cholestyramine (Questran)
Other Antacids
These medications form a barrier that floats on top of the stomach contents to prevent reflux. An example is Gaviscon, Carafate.
Surgical Treatment
Surgical Procedures often times have significant reduction of GERD symptoms and reduce long term risks of damage to the esophagus and cancer. Often, patients can get off of long term use of PPIs and avoid the long term negatives of being on that medication for years.
Surgery is considered
Surgical options include:
Hiatal Hernia Repair
Many patients with frequent of severe Reflux have a Hiatal Hernia. This is a condition where your stomach pushes up through the diaphragm and into the chest cavity. This often causes reflux symptoms and feelings of food getting stuck.
Surgical repair of a hiatal hernia brings the stomach back down into the abdominal cavity and tightens the muscles of the diaphragm around the esophagus
Hiatal Hernia Repairs can be performed alone and can be performed with a fundoplication or a bariatric (weight loss) operation
Fundoplication
This is a very common surgical treatment for GERD. It involves wrapping the top of the stomach (Fundus) around the lower esophagus to strengthen the LES and prevent reflux.
Surgery that helps reduce weight, and more importantly fat cells, to help you be healthier in many ways
Losing weight and getting healthier often can help reduce or eliminate GERD symptoms, especially when combined with a hiatal hernia repair, as mentioned above.
Endoscopic Procedures
For some patients, minimally invasive endoscopic procedures can help reduce GERD symptoms without surgery:
Surgery does entail an amount of risk including but not limited to: infection, bleeding, incomplete effects on GERD symptoms or symptom/hernia recurrence, damage to other areas/organs, anesthesia complications, and death.
Complementary and Alternative Therapies

Monitoring and Follow-up Care
For those with chronic GERD, ongoing management is important. Regular check-ups with a healthcare provider can help monitor the condition, evaluate for complications (like Barrett’s esophagus), and adjust treatment plans as necessary.
When to Seek Medical Help
If you experience any of the following symptoms, it’s important to seek medical attention:
Combination Therapy: Many patients benefit from combining medication and lifestyle changes for more effective management.
What Happens When You Make an Appointment with the GHP GERD Clinic?
We will set up an initial consultation with a provider
Common Testing Options (If Applicable)
Surgical Consultation (if applicable)
Schedule a Consultation with our Anti-Reflux Specialists now!